Conversations around “winter vomiting bugs” like norovirus typically wane during summer. However, a recent report of a norovirus outbreak in a Dublin hospital is a crucial reminder that this highly contagious virus can strike any time of year. Coupled with an outbreak of COVID-19, the immediate decision to restrict access to hospital visitors will help protect patients, their families, and hospital staff. Being informed and proactive is essential in preventing the spread of viruses, especially in environments where close contact and communal living are unavoidable.
Understanding Norovirus
Norovirus is a leading cause of gastroenteritis worldwide. Characterised by symptoms such as nausea, vomiting, diarrhoea, and stomach cramps, the virus spreads easily through contaminated food, surfaces, and close contact with infected individuals (HSE.ie)
Symptoms and Transmission
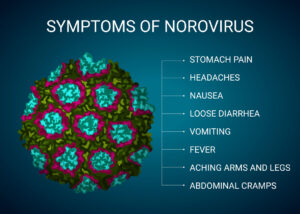
Symptoms of norovirus include:
- Nausea
- Vomiting
- Diarrhoea
- Stomach cramps
- Fever
- Headaches
- Muscle aches
These symptoms typically appear 1 to 2 days after exposure and can last 2 to 3 days. The virus spreads through direct contact with an infected person, consumption of contaminated food or water, and touching contaminated surfaces.

COVID-19
As of June 2024, there has been a noticeable increase in COVID-19 cases in Ireland. The Health Protection Surveillance Centre (HPSC) reports a rise in cases, emphasising the ongoing need for vigilance despite the advent of summer. Current data shows an increase in hospitalisations and cases across various regions in Ireland, highlighting the persistent nature of the pandemic and the importance of maintaining public health measures. (HPSC)
An interesting study that explored the impact of COVID-19 on ward transfers in Welsh hospitals found that reducing the number of non-essential inter-ward transfers significantly decreased the risk of large-scale nosocomial outbreaks. The study also detailed record-keeping as an essential tool to assess and manage the inherent risks of such movements. Improving compliance with infection prevention protocols is vital to controlling infection spread. (Patients Transfer Study)
Preventive Measures for Hospitals
- Hand Hygiene: Frequent and thorough handwashing with soap and water is critical, as hand sanitisers are less effective against norovirus.
- Isolation Practices: Isolating infected patients and using personal protective equipment (PPE) helps limit the spread.
- Cleaning Protocols: Regular and rigorous cleaning, especially on high-touch surfaces, is essential.
- Staff Training: Continuous education on infection control practices ensures that healthcare workers are equipped to handle outbreaks effectively.
- Reporting and Surveillance: Outbreak Reporting Systems should be utilised to report and monitor outbreaks, helping to understand the spread and impact on hospital resources.
Infection Prevention Protocols
The emphasis on rigorous infection prevention protocols within healthcare settings must be balanced, especially in the context of preventing infection. It is paramount to ensure the use of products and disinfectants that are approved by appropriate governmental agencies, such as HPRA, Ireland, the U.S. Environmental Protection Agency (EPA), or equivalent bodies in other countries.
Products such as Kersia Healthcare’s Klorsept and Klorkleen are rigorously tested and verified to meet specific safety and efficacy standards against pathogens.
Proper application of approved disinfectants and adherence to sanitation protocols reduce the microbial load in the environment and minimise the risk of transmission between patients and healthcare staff.
The smallest actions can have the most significant impacts!
In healthcare settings, maintaining personal hygiene and adhering to stringent infection prevention practices are crucial for the well-being of both patients and staff. Proper handwashing, use of personal protective equipment, and regular sanitisation of facilities help significantly reduce the risk of hospital-acquired infections. These practices are about compliance and cultivating a culture of safety and care.
By prioritising hygiene and infection control, healthcare facilities can protect vulnerable populations, enhance patient outcomes, and ensure a safer environment. Remember, in healthcare, the smallest actions can have the most significant impacts on health and safety.
Contact our team of experts for more information on our range of infection-prevention products suitable as a non-rinse food contact sanitiser, right up to a high-level hospital-grade disinfectant that kills pathogens like C.diff in four minutes.
USA: Chris Butler
Europe & ROW: Doireann O’Brien Kate Devereux


