Understanding Candida auris
Candida auris, a multidrug-resistant fungal pathogen, has emerged as a global health concern due to high mortality rates and resistance to commonly used antifungal drugs. First identified in 2009, C. auris has rapidly spread across healthcare facilities worldwide, leading to severe infections and increased mortality rates. This article aims to shed light on the alarming rise in death rates associated with Candida auris infections and its challenges to global healthcare systems. A recent Centres for Disease Control and Prevention (CDC) research letter analysed C.auris hospital admissions between 2017 and 2022. It estimated that one-third of mortality rates were linked to the pathogen. The most common C.auris infection was proportionate to patients with complex medical conditions.[1]
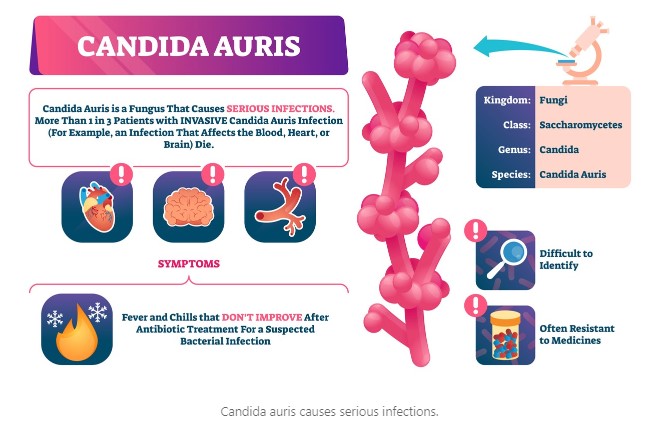
C.auris is a yeast species that can cause invasive infections, particularly in individuals with weakened immune systems or those hospitalised for long periods. It belongs to the Candida family, which also includes other common pathogens causing candidiasis, such as Candida albicans. However, what sets C. auris apart is its resistance to multiple antifungal medications, making it difficult to treat and control.
4 Factors Contributing to High Death Rates
Limited treatment options: One of the main reasons for the high mortality rates associated with C. auris infections is the limited efficacy of antifungal drugs. Traditional antifungal treatments, such as fluconazole, are often ineffective against C. auris. In contrast, other antifungal medicines, like amphotericin B and echinocandins, may have limited success rates or face the challenge of drug resistance.

Difficulty in identification: C. auris can be challenging to identify through conventional laboratory methods, leading to delayed diagnosis and initiation of appropriate treatment. This delay can exacerbate the infection, increasing mortality risk, especially in critically ill patients. It has a propensity for spreading within healthcare settings, leading to outbreaks and increased mortality rates. Its ability to persist on environmental surfaces and equipment contributes to its transmission. It can remain viable on plastic for up to 14 days and on moist surfaces for seven days. Furthermore, C. auris can colonise individuals’ skin and mucosal surfaces, making it difficult to eradicate and control within healthcare facilities.
C. auris infections primarily affect individuals with underlying health conditions, compromised immune systems, or those undergoing invasive medical procedures. These patients are already susceptible to infections, and this pathogen further exacerbates their health conditions, increasing the likelihood of adverse outcomes, including death.
Addressing the Challenge
Improved laboratory methods for the identification are crucial to enable early detection and prompt implementation of infection control measures. The development of rapid diagnostic tests specific to C. auris can significantly aid healthcare professionals in managing infections effectively. Stringent infection prevention and control practices, including proper hand hygiene, environmental cleaning, and equipment disinfection, are essential in limiting transmission within healthcare settings. Isolation protocols and strict adherence to infection control guidelines help prevent outbreaks and reduce the associated mortality rates.
Given the limited treatment options, judicious use of antifungal medications becomes critical. Antifungal stewardship programs can help optimise antifungal therapy, minimise the emergence of drug resistance, and improve patient outcomes. Continued research into the biology, pathogenesis, and mechanisms of antifungal resistance in Candida auris is necessary to develop new treatment options and strategies for combating this resilient pathogen. Investment in developing novel antifungal drugs is crucial to address the growing threat.
This pathogen represents a formidable challenge to global healthcare systems, leading to continued mortality rates due to its multidrug resistance and ability to cause invasive infections. Timely diagnosis, effective infection control measures, and the development of new treatment options are vital in reducing the impact of C.auris. Collaborative efforts among healthcare providers, researchers, and policymakers are essential to address the rising death rates associated with it and protect vulnerable patient populations from this emerging global health threat.

Precautionary Measures for Healthcare Facilities
Aggressive infection control protocols are required to prevent this and similar pathogens to spread.
- Use EPA-listed products. The product master label will state it has EPA-approved claims against C.auris.
- Ensure that your disinfectant also has the EPA claim against biofilm.
- Daily terminal cleaning and disinfection of patient rooms and care areas is essential. Special attention to the cleaning and disinfection of high-touch surfaces and shared equipment and tools.
- Consult infection prevention experts, who will help you with optimised training, protocols, and products like our KK2 effervescent tablets. EPA-approved to penetrate biofilm and eliminate the pathogens it protects.
- Build a team of infection preventionists who can monitor the outcomes of your disinfection protocols and adjust where necessary.
Read a peer-reviewed article on the efficacy of our KK2 effervescent NaDCC disinfection tablet for cleaning and disinfection here:
Get in touch with us here:
Mob: + 206 741 5981
e-mail: dan.mueller@kersia-group.com
Ref:
[1] Benedict K, Forsberg K, Gold JAW, Baggs J, Lyman M. Candida auris‒associated hospitalizations, United States, 2017–2022. Emerg Infect Dis. 2023 Jul https://doi.org/10.3201/eid2907.230540
© KersiaHealthcare 2023

